In this article:
- Difficulties studying abortion and infertility
- Planned Parenthood on abortion and infertility
- Medical organizations on abortion and infertility
- Abortion complications that cause infertility
- Abortion and miscarriage
- Abortion alternatives
- Infertility treatments and support
Many wonder, “can abortion cause infertility?” The short answer is yes, it can. There are cases where women become infertile after the procedure. There is also evidence showing that it can increase risk of future miscarriage. However, the exact probability of either is unclear, given the mixed results of studies. This is likely due to the difficulties of studying such personal and controversial issues.
It’s important to note that abortion itself may not necessarily cause infertility. However, potential complications from the procedure are known causes of infertility.
Planned Parenthood and other medical sources say that the risk of infertility is rare unless there are complications—and this last phrase is key. Planned Parenthood and other medical organizations downplay the risks of abortion, but much evidence suggests that those risks are very real. Complications are more common than they wish to admit. Such complications sometimes even resulting in death.
Difficulties in Studying Abortion and Future Pregnancies
Before we delve into the specific complications and what the data says, we must first review why it is difficult to study this particular issue.
There are many reasons why studies on abortion and infertility have mixed results.
First of all, infertility itself is difficult to study. It is a personal issue often not discovered until a couple tries to conceive, and sometimes not even until months or years of trying. It is also difficult to diagnose causes of infertility since there are so many factors at play.

Secondly, abortion is even more difficult to study, since many women are hesitant to admit to having one. Because of this, three major issues arise:
-Many studies have too few post-abortive subjects to be accurate.
-In other studies, the statistics are affected because women did not admit to having the procedure.
-If the patient’s doctor isn’t informed that the abortion happened, the doctor won’t even know to consider it as a cause of infertility.
Additionally, because there is a lack of abortion follow-up care, many women are unaware of its effects on their health and fertility. In one case study, the doctors found that the patient’s infertility was due to bone fragments left from an incomplete abortion. However, the patient had no idea there had been any complications. Nor did the doctor realize it at first because they were unaware that the woman had had an abortion, and the first scans didn’t find any evidence.
These factors make it difficult for anyone to realize the full truth.
Finally, those who support abortion may be influenced by political concerns. As Gregory K. Pike (Senior Research Fellow at the Bios Centre in London) says in his research: “it is quite conceivable that the literature as it exists is biased.”1
Many ask whether abortion will cause miscarriages in the future. As with fertility, miscarriages can happen for a multitude of reasons. Thus, measuring why a particular miscarriage happens can prove difficult, if not impossible. This muddies certainty on whether abortion directly causes future miscarriage. That being said, there are complications that can cause miscarriages in the future. We will discuss these below.

What Planned Parenthood Says
Planned Parenthood claims that there is no increased risk of infertility from abortion “unless there’s a rare and serious complication that’s not treated.” But such complications are not always treated.
In his overview of studies on abortion and infertility, Pike responds to Planned Parenthood:
This implies that complications serious enough to affect fertility are rare (0.01% to 0.1%…2), and only present a problem if untreated. However, some quite serious abortion complications are not rare (e.g. blood transfusions required in up to 0.6% of [chemical] abortions, and [pelvic inflammatory disease] in up to 4.9% of surgical abortions).3
While this still is not very common, it’s quite possible that these statistics are even higher given the previously-mentioned issues in studying this topic. In other words, the risks of serious complications from abortion are higher than supporters would like to admit.
What Medical Organizations Say About Infertility and Abortion
Other medical organizations admit there may be some risks of infertility, though in the end they generally downplay these risks. They say that there isn’t enough evidence to claim a definite connection. Some even expressly state that there is no risk, against evidence to the contrary.
For example, many medical organizations mention a small risk from abortion complications, such as infections and scarring of the uterus. The NHS says that “most infections are treated” before they lead to pelvic inflammatory disease (PID). Though, as mentioned previously, PID still occurs in almost 5% of surgical abortions (and those are only the recorded cases). Thus, there’s still a good amount of women having abortions who end up developing PID. (For reference, 5% of surgical abortions in 2020 totals about 10,440).
Mayo Clinic and the British Pregnancy Advisory Service also admit that studies show “a link between prior surgical abortion and a slight increased risk of premature birth and low birth weight,” risks which increase with each abortion.
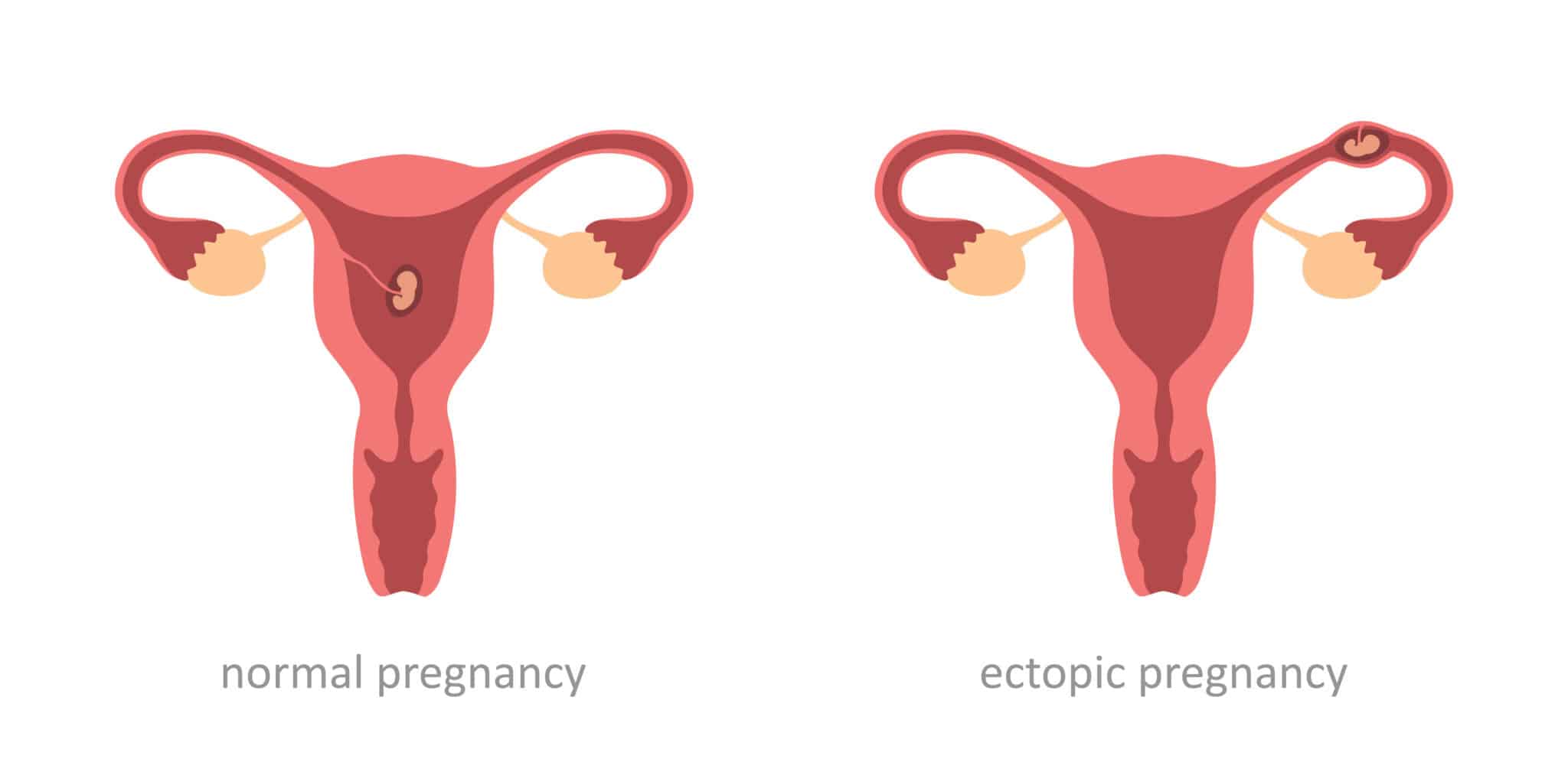
After all this, though, they still argue that “there is no proven connection between abortion and future infertility, ectopic pregnancy or other pregnancy complications.”
Admittedly, there are not enough studies on abortion and infertility (for the reasons mentioned above), and those that exist are not always reliable. Nonetheless, there is evidence of at least some risk. There are recorded cases of women who became infertile because of the complications. And some abortion complications are known causes of infertility, as we shall see. Thus, as Pike argues, there is a “variety of reasonable grounds for a link” between abortion and infertility.
In other words, what is important to note is that abortion can affect future fertility. While this fact is often admitted by pro-abortion sources, it is often downplayed (if it’s admitted).
Abortion Procedures and Future Fertility
Research shows that whether abortion affects future pregnancies seems to depend on the type of abortion procured.
Medical abortion (MC) is when the mother takes a drug to induce an abortion (typically mifepristone and/or misoprostol). Surgical abortion (SA) is when the child is removed from the uterus through the vagina, often using suction or forceps with a curet to scrape the walls of the uterus to ensure all pieces are removed.
Some complications that can result from an SA seem to stem specifically from scraping the walls of the uterus with a curet. This can cause infertility, miscarriages, premature birth, and low birth weight (discussed below). The dilation of the cervix during SAs can also cause cervical injury, leading to future miscarriages. SAs seem to affect future fertility more than MAs, though we will see that MAs can also pose a risk to cervical health.
Complications That Can Cause Infertility
Pike’s research identifies several abortion complications:
- Cervical damage
- Infection and pelvic inflammatory disease (PID)
- Incomplete abortion
- Adhesions from damage to the uterus (Asherman Syndrome)
- Poor mental health (depression, anxiety, etc.)
Most of these are known causes of infertility. Thus, it only makes sense that there is some relationship between abortion and infertility.

Cervical Damage
The risk of cervical damage is often reported to be about 1%, while the overall risk of complications is about 2%. Cervical damage can lead to later miscarriages. Admittedly, “a link via cervical damage from abortion remains theoretical,” but “it should be the subject of further research.”4
Infection and PID
We can confidently say, however, that infection from abortion can lead to PID (pelvic inflammatory disease), and thus infertility. This applies to both chemical and surgical abortion, since “your cervix opens during an abortion and allows bacteria to enter your genital organs more easily.”
As one study notes, “Abortion clinics are often not equipped with the optimal instruments for reliable diagnosis… [to] protect patients from serious infection.” It also found that the prevalence of PID “…was 2.4% after pharmacological abortion and 4.9% after surgical abortion.”
Such infections can lead to PID if left untreated (which is quite possible given the lack of post-abortion care, and the fact that patients with PID do not always show symptoms). Based on various studies, PID is a known cause of infertility—between 10% and 40% of infertility cases.5
According to several studies done in the 80s, between 10% and 28% of women who had abortions developed PID. And this statistic would be even higher if it included cases that went undetected because of a lack of symptoms.
More recent studies affirm this connection. In a 1995 study, Stevenson et al. claim that pelvic infection is the most common complication from abortion. A 1996 case study found that 56% of women with PID had at least one abortion, and a 2007 study estimated that women with an untreated STI from abortion have a 63% chance of developing PID.
According to Pike, there is an up to 1% chance of getting infertility from abortion due to PID alone—though this number would be even higher if it included cases of asymptomatic PID.6

Incomplete Abortion
An incomplete abortion raises the risk of infection and PID and requires surgery to remove the remaining fetal parts. The surgery carries further risks of infection and damage, thus further augmenting the risk of infertility issues.
Indeed, “the retention of bone fragments after abortion has been linked to secondary infertility.”
While retained fetal parts were found in only about 0.15% of women who had a hysteroscopy (an examination of their uterus), “this might be misleading,” as a previously-mentioned case study shows. In the case study, the doctors did not identify the incomplete abortion at first, since the first scans did not find the retained fetal parts and the doctors were unaware of the past abortion. Only later did they discover that an incomplete abortion was causing the woman’s infertility.
Intrauterine Adhesions (Asherman Syndrome) and Endometrial Thinning
If the endometrial lining is damaged during an abortion, bands of scar tissue can form inside the uterus. This can cause the sides of the uterus to stick together. These bands of scar tissue are known as intrauterine adhesions (IUAs), which can cause infertility.
Although studies are inconsistent about the exact percentage, “the evidence for a link between abortion and IUAs is clear.”7 This is especially true for SAs and even more so for incomplete abortion.
“The link between IUAs and infertility is perhaps even more established.” says Pike. IUAs, “depending on the severity, may lead to infertility in up to 43% of such cases.” In another study from 2007, Kodaman and Aydin affirm that “intra-uterine adhesions can cause recurrent pregnancy loss and infertility.” Furthermore, The American Society for Reproductive Medicine says that, after treatment, the chance of pregnancy can be anywhere from 20% to 80% or lower, depending on the severity of the damage.
One 2018 study also discovered that abortion caused endometrial thinning, a higher chance of miscarriage, and a lower chance of pregnancy (though it only examined success with IVF). And the more SAs the woman had undergone, the higher the risk.
Thus, we see that IUAs “may be a hidden yet significant cause of infertility after abortion. And yet the research has been so limited that women will receive minimal if any guidance.”
Abortion and Risks of Miscarriage
After abortion, there may also be a risk of future miscarriage.
A 2023 study found that women with a history of miscarriage or abortion “…were at 2.71 times increased risk for cervical dysfunction during pregnancy.” A weakened or damaged cervix is a risk factor for miscarriage.
A study from 2003 found that “a higher risk of miscarriage, particularly those occurring within the first 3 months of gestation, is associated with prior first trimester induced abortion.” This seemed to at least be true of vacuum aspiration abortions, since the majority of the abortions in this study were done by this technique.
While the study acknowledges that “results from previous studies are conflicting,” many factors (such as small sample sizes and subjects all coming from the same hospital) make their accuracy questionable.
The researchers suspect that damage and infections from abortion may cause delay in the embryo’s implantation, thus leading to miscarriage.
Another study indicated that an MA may carry less risk of miscarriage than an SA. But it’s important to note that MAs are not immune from posing risk to the cervix: “In contrast to normal labor where the cervix is dilated slowly, the more rapid mechanical stretching of the cervix required by surgical abortion and later-term medical abortions can result in long-term cervical damage.”
As with studies on infertility and abortion, there are not enough studies on abortion and miscarriage to come to a conclusive answer. And again, the controversial and personal nature of abortion and miscarriage make the issue difficult to study.
What Alternatives Do You Have?
If you are considering an abortion, please know that there are truly viable alternatives.
And please do not hesitate to reach out for guidance and support from your local pregnancy center. And make sure you understand why abortion is wrong if you are unsure.
For those dealing with a past abortion, we know the effect it can have on your mental health. Find a support group or pro-life therapist to help you heal.

Infertility Treatments and Support
If you’ve had an abortion, don’t panic. Meet with your doctor with any concerns you have. If you or a loved one is struggling with infertility, there are many treatment options, resources, and support available to you.
For more information on ethical infertility treatments in line with Church teaching:
- Assisted Reproductive Technologies: A Catholic Perspective
- The Ethics of Artificial Reproductive Technologies
- NaProTECHNOLOGY
If you’re having difficulties becoming pregnant, consider seeking spiritual advice and encouragement:
- 5 Infertility Support Groups for Catholics
- Project Rachel
- Trusting God through Infertility
- 8 Uplifting Bible Verses for Couples Struggling with Infertility
This article was originally published in November 2022 by Emily Capps and was most recently updated in November 2023 by Marisa Cantu.
+ Endnotes
[1] Pike, G. K. (2020). Abortion and Infertility. Issues in Law & Medicine, 35(1/2), 173–195.
[2] These definitions have been determined by the Council for International Organizations of Medical
Sciences (CIOMS), an organization established by WHO and UNESCO. They are described in the CIOMS training manual, which can be found at http://www.who.mt/medicines/areas/quality_safety/safety_efficacy/trainingcourses/definitions.pdf. Accessed 28 Jun 2018.
[3] Pike, G. K. (2020). Abortion and Infertility.
[4] Pike, ibid.
[5] Also see Wiesenfeld, Harold C., Hillier, Sharon L., et al. Subclinical Pelvic Inflammatory Disease and Infertility. Obstetrics & Gynecology: July 2012. Volume 120, Issue 1, p. 37-43
doi: 10.1097/AOG.0b013e31825a6bc9
[6] “If symptomatic PID, even after antibiotic treatment, occurs at a frequency of between 2.4% and 4.9%, and infertility after PID between 10% and 20% for symptomatic cases, then in total there could be up to 1% infertility (20% of 4.9%) after abortion from PID alone. However, that figure could treble if asymptomatic PID is taken into account” (Pike, ibid).
[7] Pike, ibid.






